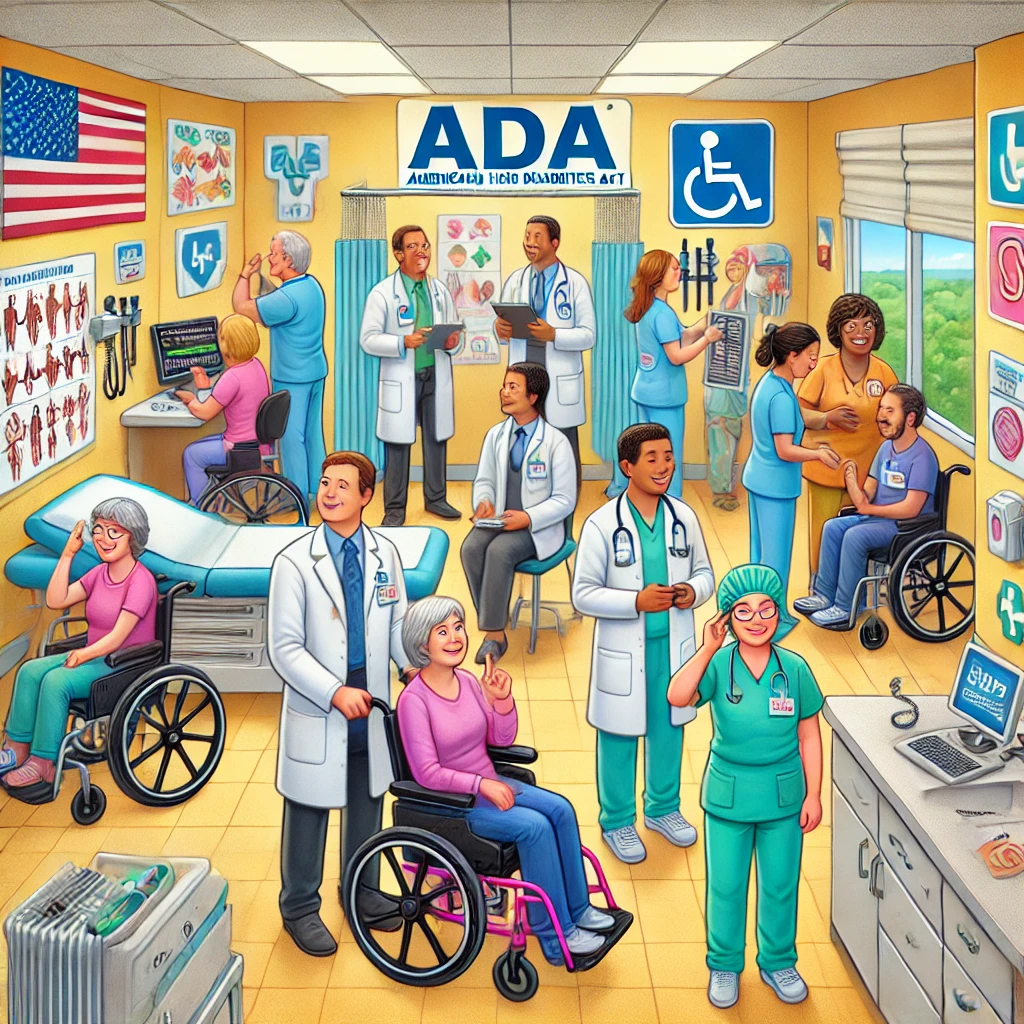
The Americans with Disabilities Act (ADA), enacted in 1990, is a pivotal civil rights law that aims to eliminate discrimination against individuals with disabilities. The ADA is crucial in various settings, with healthcare being one of the most significant. As a comprehensive piece of legislation, the ADA necessitates critical adaptations in healthcare facilities, ensuring that services are accessible and equitable for all patients, regardless of their disabilities. This article provides an in-depth look at how the ADA applies to healthcare settings, covering nuances and key focus areas.
Introduction: Ensuring Accessibility in Healthcare
Accessibility in healthcare refers to the ability of patients to obtain and make use of healthcare services. For individuals with disabilities, this accessibility is not only vital but a matter of civil rights, as stipulated by the ADA. Healthcare settings must comply with ADA regulations to offer an inclusive environment that caters to the diverse needs of all patients. This involves making modifications to facilities, ensuring effective communication, and training staff to be adequately equipped to handle the requirements of disabled patients.
Despite the ADA’s rigorous guidelines, compliance can often be overlooked or inadequately implemented. Statistics indicate that while many healthcare facilities have made strides in improving accessibility, there is still significant work to be done. The importance of ADA compliance extends beyond legal obligations; it underpins the very essence of equitable patient care. By comprehending the ADA’s requirements and integrating them seamlessly into healthcare settings, facilities can better serve their communities, fostering an environment of inclusivity and respect.
Physical Accessibility in Healthcare Facilities
Physical accessibility is one of the cornerstone requirements of the ADA in healthcare settings. This encompasses the structural design and layout of healthcare facilities, ensuring that they are usable by individuals with varying physical disabilities. Key ADA requirements include accessible entrances, ramps, bathrooms, patient rooms, and medical equipment.
Healthcare facilities must have at least one accessible entrance and route connecting all essential areas to accommodate wheelchair users and individuals with mobility impairments. Elevators should be available where multiple floors exist, and emergency exits must also be accessible. Bathroom facilities require special adaptations, including grab bars, adequate space for maneuvering, and accessible sinks and toilets.
Moreover, patient rooms and medical equipment must be designed to accommodate individuals with disabilities. This includes adjustable examination tables, accessible diagnostic equipment, and ensuring sufficient room within patient rooms for wheelchair use. The ADA stipulates these requirements to ensure that individuals with disabilities can receive the same standard of care as everyone else.
Communication Accessibility: Ensuring Effective Patient-Provider Interaction
Communication is a critical component of healthcare, and ensuring effective communication with patients who have disabilities is a mandated requirement under the ADA. This means healthcare providers must ensure that their communications with patients, family members, and companions with disabilities are as effective as those with non-disabled individuals.
For patients with hearing impairments, healthcare facilities may need to provide auxiliary aids and services, such as qualified interpreters, real-time captioning, or hearing aid-compatible telephone systems. Written materials should be available in alternative formats, such as Braille, large print, or accessible digital formats, to accommodate patients with visual impairments.
Additionally, healthcare professionals should be trained to communicate effectively with individuals with intellectual or developmental disabilities. This may involve using simple language, visual aids, and ensuring that patients fully understand their medical conditions and treatment options. Effective communication ensures that all patients can participate actively in their healthcare decisions, thereby improving health outcomes and patient satisfaction.

Non-Discrimination Policy and Training
The ADA not only mandates physical and communication accessibility but also requires healthcare facilities to adopt and enforce non-discrimination policies. These policies must explicitly state that discrimination based on disability is prohibited, and must be communicated to all staff members and patients.
Training is a crucial aspect of implementing an effective non-discrimination policy. Healthcare providers, administrative staff, and other personnel should receive comprehensive training on the ADA’s requirements and the facility’s commitment to accessibility and non-discrimination. This training should cover recognizing and addressing different types of disabilities, understanding legal obligations, and learning best practices for interacting with and accommodating patients with disabilities.
By fostering a culture of inclusion and respect, healthcare facilities can ensure that all patients, regardless of their abilities or disabilities, receive high-quality care. This commitment not only fulfills legal obligations but also enhances the reputation and credibility of the healthcare provider.
Reasonable Modifications and Accommodations
Under the ADA, healthcare facilities are required to make reasonable modifications to policies, practices, and procedures to accommodate individuals with disabilities. Reasonable modifications are adjustments or changes that enable disabled individuals to receive medical services on an equal basis with others.
Examples of reasonable modifications include allowing a service animal to accompany a patient in the hospital, providing extra time during appointments for patients with cognitive impairments, or altering appointment scheduling processes to accommodate patients with mobility issues. These modifications are essential to ensure that the services are equitable and that patients with disabilities are not disadvantaged.
Healthcare providers must also be prepared to make individual assessments of accommodation requests. Each request should be considered on a case-by-case basis, taking into account the specific needs of the patient and the feasibility of the modification. The goal is to provide accommodations that are reasonable without fundamentally altering the nature of the healthcare services provided.
Enforcement and Compliance Mechanisms
Compliance with the ADA is not optional; it is legally mandated. There are various mechanisms in place to enforce compliance and address violations. Patients who believe their rights under the ADA have been violated can file complaints with the U.S. Department of Justice (DOJ) or the Office for Civil Rights within the Department of Health and Human Services (HHS).
These agencies investigate complaints and have the authority to take action against healthcare providers that fail to comply with the ADA. This can include requiring corrective measures, imposing fines, or even initiating lawsuits where necessary. Healthcare facilities must therefore maintain thorough records of their compliance efforts, including documentation of physical and communication accessibility measures, non-discrimination policies, training programs, and reasonable modifications made.
Regular self-assessment and auditing are recommended practices for healthcare providers to ensure ongoing compliance with the ADA. By proactively identifying and addressing potential areas of non-compliance, healthcare facilities can avoid legal issues and continue to provide accessible, inclusive care to all patients.
Conclusion: The Ongoing Commitment to Accessible Healthcare
The Americans with Disabilities Act has transformed the landscape of accessibility in healthcare settings, promoting a more inclusive and equitable approach to patient care. While significant progress has been made since the ADA’s enactment, the journey towards full compliance and accessibility is ongoing. Healthcare providers must recognize their critical role in this journey and remain steadfast in their commitment to upholding the civil rights of individuals with disabilities.
Meeting the ADA’s requirements involves a multifaceted approach, encompassing physical and communication accessibility, non-discrimination policies, reasonable modifications, and rigorous training and compliance measures. Each of these elements is essential to ensure that individuals with disabilities can access healthcare services without facing barriers or discrimination.
Ultimately, compliance with the ADA is more than a legal obligation; it is a moral imperative that reflects the values of equity, dignity, and respect for all individuals. By continuously striving to create accessible healthcare environments, providers can foster trust, improve patient outcomes, and contribute to a more just and inclusive society.
As the healthcare industry continues to evolve, ongoing dedication to ADA principles will be crucial in addressing the diverse needs of patients and ensuring that everyone has the opportunity to receive the care they deserve.
Frequently Asked Questions
1. What is the purpose of the Americans with Disabilities Act (ADA) in healthcare settings?
The ADA, enacted in 1990, serves as a groundbreaking civil rights law designed to eliminate discrimination against individuals with disabilities, including in healthcare settings. The primary aim of the ADA within healthcare environments is to ensure that all services and facilities are accessible and equitable for everyone, regardless of their abilities or disabilities. This means healthcare facilities must make necessary accommodations and adjustments to ensure individuals with disabilities can access the same level of care as others. For instance, this might involve installing ramps and elevators for individuals using wheelchairs, providing sign language interpreters for patients who are deaf, or offering written materials in braille or large print for those with visual impairments. Ultimately, the ADA champions the rights of individuals with disabilities, advocating for equal opportunities and full participation in all aspects of society, including healthcare.
2. How does the ADA impact the physical design and layout of healthcare facilities?
The ADA has a significant impact on the architectural design and layout of healthcare facilities by mandating certain standards that ensure accessibility for individuals with disabilities. These standards often call for modifications to both the interior and exterior of these facilities. For the exterior, this includes the provision of accessible parking spaces with sufficient room for mobility devices, pathways without obstructions, ramps, and curb cuts for easy entry and movement. Inside facilities, doorways must be wide enough to accommodate wheelchairs, and restrooms should be equipped with grab bars and accessible stalls. Examination rooms, patient service counters, and waiting areas must also be designed to provide enough space for maneuvering wheelchairs. Additionally, the installation of visual alarm systems benefits individuals who are deaf or hard of hearing. By adhering to these structural requirements, healthcare providers ensure that all patients can independently access necessary medical services.
3. What responsibilities do healthcare providers have under the ADA to ensure effective communication with patients with disabilities?
Healthcare providers have a fundamental responsibility under the ADA to ensure effective communication with patients with disabilities, tailoring accommodations to each patient’s unique needs. This involves providing auxiliary aids and services such as sign language interpreters for individuals who are deaf, providing written notes or real-time captioning services, or supplying text telephones (TTY) equipment for effective communication over the phone. For patients with speech impairments, the use of speech-to-text devices may be necessary. Moreover, printed information, including consent forms, prescriptions, or educational materials, should be available in accessible formats like large print, braille, or electronic versions that screen readers can interpret. The goal is to eliminate any communication barriers that might impede a patient’s understanding of their medical condition or treatment options. Through robust communication support, healthcare providers not only comply with the ADA but also enhance the quality of care by fostering a more inclusive environment where all patients feel valued and empowered to engage actively in their healthcare decisions.
4. What are some common challenges healthcare facilities face with ADA compliance, and how can they address these issues?
Healthcare facilities frequently encounter several challenges when attempting to comply with ADA requirements, primarily due to the complexities involved in modifying existing structures and adapting services. One common challenge is retrofitting older buildings that were not originally designed with accessibility in mind. This might involve costly modifications such as expanding doorways, installing elevators or ramps, and updating restroom facilities. Financial constraints can also hinder efforts to implement necessary changes promptly. Facilities may address these issues by prioritizing modifications based on the needs of their patient population and seeking grants or funding specially allocated for ADA compliance projects. Additionally, training staff on the importance of ADA compliance and effective communication strategies can help address gaps in service delivery. Proactive planning and regular audits can ensure facilities remain compliant with changes in ADA guidelines and continue to provide accessible care to all patients.
5. How does ADA compliance benefit healthcare facilities beyond mere legal adherence?
Beyond fulfilling legal requirements, ADA compliance offers numerous benefits to healthcare facilities. First and foremost, it promotes inclusivity, ensuring that all patients, including those with disabilities, can access quality healthcare services. This inclusivity can enhance the reputation of facilities as compassionate and patient-centered institutions, attracting a broader patient base. Moreover, by facilitating better communication and accessibility, ADA compliance often leads to improved patient satisfaction and health outcomes, as patients are more likely to understand and adhere to treatment plans. Additionally, accommodating employees with disabilities can expand the talent pool, bringing diverse perspectives and capabilities into the workforce. Financially, while initial costs may seem significant, compliance can mitigate the risk of costly legal challenges associated with discrimination claims, thus protecting the facility’s resources and reputation. Overall, ADA compliance is not just a legal obligation but a strategic advantage that aligns with the principles of equity and human rights.